The carcass and all materials associated with the carcass should be destroyed and the ground should be disinfected. This can be very difficult. The preferred method of destruction is incinerating the carcass. If incineration or cremation is not possible, burying the carcass deep (at least 6 feet) is acceptable.
■ The following are general recommendations for burning
a 1,000-pound carcass:
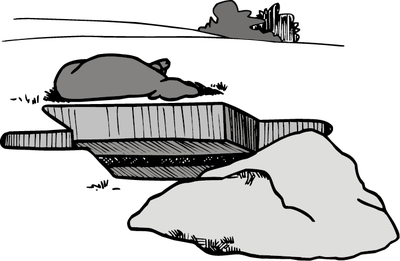
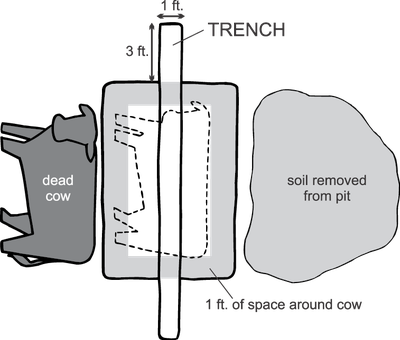
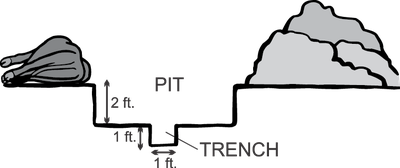
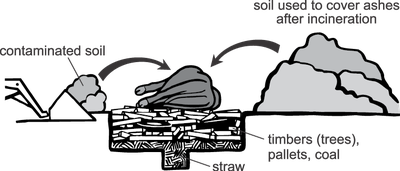
Dig a pit about 2 feet deep and exceeding the length and breadth of the carcass by about 1 foot on each side (Figure A). Dig a trench 1 foot by 1 foot along the length of the center of the pit, extending beyond the ends of the pit by about 3 feet; this serves as an air duct for the fire under the carcass (Figure B). Fill the trench and cover the bottom of the pit with straw and soak it with an accelerant (kerosene or diesel fuel (Figure C).
Top view.
Cross section.
Cross section of pit ready for burning.
Wood, such as trees or pallets that have been cut to fit across the trench and within the sides of the pit, then should be placed on top of the straw. Add other pieces of wood (or coal) until the pit is filled to the level of the ground surface. Saturate all of this with accelerant.
If you have questions regarding what other types of materials are acceptable to use in the burn, contact the North Dakota Department of Environmental Quality, Division of Air Quality at 701-328-5188.
The carcass can then be lifted or drawn onto the pyre (combustible heap). Pour further accelerant over the carcass. Ignite the fire at either end of the trench. Once the incineration is well under way (probably after the first hour), cover the pyre with corrugated metal or other metal sheeting to retain heat but not lose ventilation.
If blood and body fluids have contaminated the ground and material under the animal, they should be incinerated as well. Remove soil deep enough to collect any blood and body fluids that have seeped into it. This could be up to 6 inches.This material can be placed on top of the carcass prior to igniting the pyre (Figure C).
The approximate quantities of fuel that will be needed are 100 pounds of straw, 2½ gallons of accelerant and 2 tons of wood or ½ ton of wood and ½ ton of coal.
If soil and other related materials cannot be incinerated, they can be disinfected with a 5% formaldehyde solution at 50 quarts per square yard.
After incineration, cover ashes and contaminated soil with soil removed from the pit.